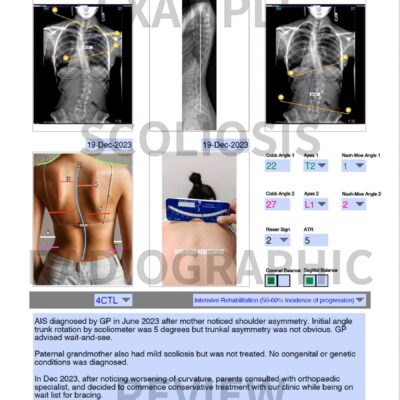
X-ray (Radiographic) Overview
X-ray (radiography) is a important diagnostic and monitoring tool in the care of scoliosis. It allows health professionals to diagnose pathologies and congenital abnormalities, measure Cobb angle(s), spinal balance, identify specific curve patterns (exercise prescription and brace design depend on this), and monitor curvature changes over time.
The following is an overview of scoliosis radiography from a clinician’s perspective. For an example of how it is used clinically, please refer to our X-ray review.
Essential Views
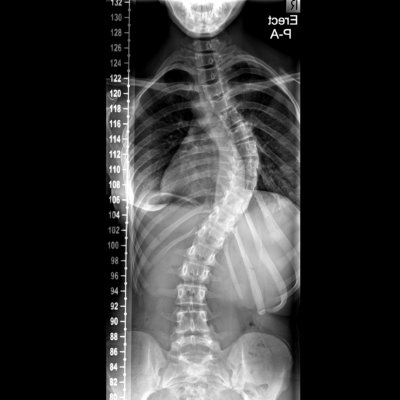
To confirm the diagnosis of scoliosis, typically we require two views of the vertebral column, known as a "scoliosis series". One is a full-spine, standing AP (anterior to posterior) or PA (posterior to anterior) view. The AP projection is also known as the frontal view. The other one is the lateral view or sagittal view.
AP or PA View
The full-spine, AP or PA view provides a comprehensive assessment of spinal alignment, major curvatures, rotational deformities, allows the measurement of Cobb angle(s) and coronal balance.
The choice of AP or PA projections depends somewhat on the preference of the requesting physician or radiographer. For the purpose of scoliosis evaluation, the PA projection is preferred. It has the advantage of minimising distortion of the thoracic spine as the vertebrae are closer to the X-ray machine than the AP projection. It also keeps the sensitive soft tissue (breasts and gonads) further away from the source of radiation.
In subsequent check-ups, typically just the full-spine (either AP or PA) view is necessary. In between, observation and physical measurement with a scoliometer are used to monitor progress.
Radiographic positioning
The radiograph should include both iliac crests to show pelvic tilt, and better yet, both acetabula showing the femoral heads, and up to and include entire C7 vertebral body. The patient should be in mid-breath (between breath in and breath out).
Lateral (Sagittal) View
The full-spine, lateral or sagittal view offers important insight in the dynamic function of the spine. In adult scolioses, tilting, pathological processes including Schmorl’s nodes and osteoporotic fractures are well visualised in the lateral view. It also allows the measurement of sagittal balance.
Furthermore, certain features on the lateral view can be an indicator for specific exercise techniques. We frequently see patients with scoliosis with a loss of thoracic kyphosis (flattening of the normal round curve in the upper back) and/or a loss of lumbar lordosis (a straightening of the normal arch in the lower back). Occasionally, scoliosis patients may also present with hyperlordosis (excessive arch of the lower back).
Schroth therapists teach patients to perform certain exercises (e.g. cat walk) to address the sagittal plane abnormality with the goal to establish a normal thoracic kyphosis and lumbar lordosis. In continuation the motional segments work together so the spine functions like a coiled spring to allow absorption and transmission of kinetic energy with movement.
Radiographic positioning
The radiograph should include the hip joint, and up to and include entire C7 vertebral body and posterior and superior edge of S1, with the patient’s arms flexed at 90 degrees. The patient should be in mid-breath (between breath in and breath out).
Supplementary Views
Lateral (side) bending views
Other than the two views in a standard “scoliosis series”, sometimes lateral (side) bending views may be obtained to assess the amount of side bending available. If the range of motion is limited in thoracic joints or between ribs (by comparing side bending and PA views), certain movements (e.g. lateral shift in muscle cylinder exercise) should be prioritised.
It is also referenced by orthotists (brace maker) when deciding where to apply corrective force, and used by surgeons to assess the area(s) with the greatest stiffness (known as the primary or structural curve) when considering surgical fixation.
Radiographic positioning
The patient is erect or supine. The patient bends his/her upper body laterally (right and left) from the hips as much as possible. The radiographer ensures rotation of hips and shoulders is at a minimum, and at least 3-5 cm of iliac crests are present on the radiograph.
Frequently Asked Questions
How often do I need new X-rays?
For adolescents, the frequency may range between every 3-12 months depending upon initial curve severity, age of discovery, expected curve progression, and skeletal maturity (Risser Sign). For adults with scoliosis, less frequent monitoring is required as the spine is more stable. However, if pain (especially new pain) is present, a new set of X-rays should be requested.
Will cancer risk increase due to excess radiation?
While radiation exposure is a legitimate concern, patients undergoing X-ray examination (even cumulatively) receive effective doses significantly lower in comparison with other forms of radiographic examination.
Precautions and protection
It is better to have X-rays at a facility with modern digital equipment because newer systems minimise exposure by using better detectors and software manipulation to enhance images.
Since soft tissue is more susceptible to radiation, ask the technician to provide a lead apron to shield the breasts and the ovaries/genitals where possible.
If you as a parent or patient, are highly concerned about radiation risk, look for an electro-optical sensor (EOS) imaging centre. EOS is said to offer better image quality with significantly reduced exposure when compared to conventional X-ray.
What is the likelihood of the scoliosis getting worse?
In general, the earlier the age in which scoliosis is diagnosed, the greater the Cobb angle(s) at the time of diagnosis, the greater the likelihood of a severe scoliotic curve. This is why early diagnosis and pro-active therapy (not wait-and-see!) are so important. The likelihood of curve progression can be calculated using the Lonstein formula (Karavidas NS 2016), which is part of our X-ray review.
Scoliosis X-ray (Radiographic) Terminology
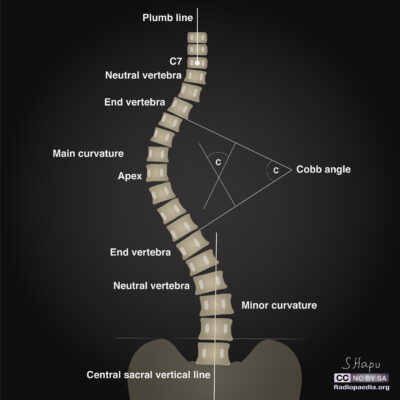
Apex or apical vertebra(e)
The apex is the crest of the curve. There may be one apex if the scoliosis is of a C shape and two apices if there are two continuous curves wherein the spine appears as an S shape. Technically, the apex is the vertebra or disc space which is furthest away from the expected centre of the vertebral column, and/or shows the greatest rotation of the vertebral body.
End vertebra(e)
The end vertebra(e) are on either ends of a scoliotic curve. An imaginary line from the upper end plate of the superior end vertebra, and the other imaginary line from the lower end plate of the inferior end vertebra, intersect to form the Cobb angle.
Neutral vertebra(e)
Neutral vertebrae are present on either side of the apical vertebrae which demonstrate no rotation (around an imaginary vertebral axis), typically a few segments away from each end vertebra.
Stable vertebra
The stable vertebra is the first vertebra below the lowest curve which is roughly bisected by the central sacral vertical line (CSVL).
Vertebral body rotation
Several methods are used to estimate vertebral body rotation on radiographs. The widely used Nash-Moe method, uses the pedicle position on frontal radiographs as an indicator of the extent of vertebral body rotation (click on the second picture on the left to see the illustration). The vertebra on the convex side of scoliotic curve is divided into two equal halves, and each half into three equal segments. Vertebral body rotation is quantified on the basis of the pedicle location in regard to the three segments (Grades 1-4). There is some correlation between vertebral body rotation on seen radiographs to angle of trunk rotation when performing the Adam’s forward bending test, as measured using the scoliometer.
Measuring spinal balance
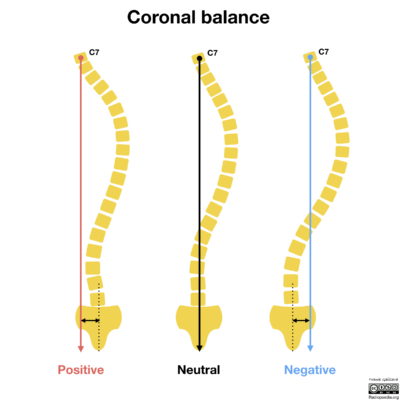
Coronal balance
Coronal balance provides an indication whether the spine is balanced between two sides of the vertebral column or is tilted to one side. Imbalance suggests an uneven distribution of load and hence a greater likelihood for degenerative changes and/or curve progression in a scoliosis patient.
Measurement
A plumb line is drawn down from the mid-point of the C7 vertebral body, on a weight bearing full-spine radiograph without side bending. The horizontal distance between this plumb line and the midline of the sacrum or central sacral vertical line (CSVL) should be less than 2cm, exceeding this is considered off balance.
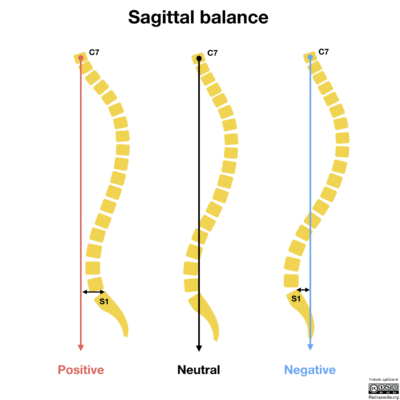
Sagittal balance
Sagittal balance provides an indication of weight and stress distribution through the axial skeleton. It forms part of the radiographic assessment of spinal deformity including kyphotic disorders and scoliosis.
Measurement
Several methods are used to measure sagittal balance for different purposes. One of the simplest and most widely used methods is the C7 plumb line. The measurement is taken on a lateral standing full-spine radiograph. A plumb line is drawn from the middle of the body of the C7 vertebral body. This line should pass through the posterior and superior corner of the S1 vertebral body. If the horizontal distance between the plumb line and the S1 corner is more than 2 cm, it is considered off balance.